Abstract and Introduction
Abstract
Calcium supplements have been widely used by older men and women. However, in little more than a decade, authoritative recommendations have changed from encouraging the widespread use of calcium supplements to stating that they should not be used for primary prevention of fractures. This substantial shift in recommendations has occurred as a result of accumulated evidence of marginal antifracture efficacy, and important adverse effects from large randomized controlled trials of calcium or coadministered calcium and vitamin D supplements. In this review, we discuss this evidence, with a particular focus on increased cardiovascular risk with calcium supplements, which we first described 5 years ago. Calcium supplements with or without vitamin D marginally reduce total fractures but do not prevent hip fractures in community-dwelling individuals. They also cause kidney stones, acute gastrointestinal events, and increase the risk of myocardial infarction and stroke. Any benefit of calcium supplements on preventing fracture is outweighed by increased cardiovascular events. While there is little evidence to suggest that dietary calcium intake is associated with cardiovascular risk, there is also little evidence that it is associated with fracture risk. Therefore, for the majority of people, dietary calcium intake does not require close scrutiny. Because of the unfavorable risk/benefit profile, widespread prescribing of calcium supplements to prevent fractures should be abandoned. Patients at high risk of fracture should be encouraged to take agents with proven efficacy in preventing vertebral and nonvertebral fractures.Introduction
In 2001, a National Institutes of Health (NIH) Consensus Development Panel on osteoporosis concluded that calcium intake is crucial to maintain bone mass and should be maintained at 1000–1500 mg/day in older adults [NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis and Therapy, 2001]. The panel acknowledged that the majority of older adults did not meet the recommended intake from dietary sources alone, and therefore would require calcium supplementation. Calcium supplements are one of the most commonly used dietary supplements, and population-based surveys have shown that they are used by the majority of older men and women in the USA [Bailey et al. 2010; Xiao et al. 2013]. In the last decade, several large randomized controlled trials (RCTs) of calcium supplements have been reported, and their results have led to concerns about fracture efficacy and safety of calcium. Five years ago, we reported that calcium supplements increased the rate of cardiovascular events in healthy older women and suggested that their role in osteoporosis management be reconsidered [Bolland et al. 2008]. More recently, the US Preventive Services Task Force recommended against calcium supplements for the primary prevention of fractures in noninstitutionalized postmenopausal women [Moyer, 2013]. Here, we review the evidence underpinning this substantial shift in recommendations, over only 12 years. We briefly review the data on fracture efficacy with calcium supplements, and then review the evidence for adverse effects of calcium, with a particular focus on cardiovascular risk.Fracture Efficacy of Calcium
In a population of institutionalized older women with low dietary calcium intake and a very high prevalence of vitamin D deficiency, coadministered calcium and vitamin D (CaD) significantly reduced the risk of hip and nonvertebral fracture [Chapuy et al. 1992]. However, the evidence for benefit on fracture from either CaD or calcium monotherapy in community-dwelling populations is less robust, although calcium supplements reduce bone turnover and slow bone loss [Reid et al. 2006]. Three large RCTs did not show reductions in the risk of fracture with calcium monotherapy [Grant et al. 2005; Prince et al. 2006; Reid et al. 2006]. In meta-analyses including these RCTs, calcium monotherapy marginally reduced the risk of total fracture [nine trials, n = 6517, relative risk (RR) 0.90, 95% confidence interval (CI) 0.80–1.00] [Tang et al. 2007], but increased the risk of hip fracture [Bischoff-Ferrari et al. 2007; Reid et al. 2008], although this finding was based on relatively small numbers of hip fractures. The addition of vitamin D to calcium supplements did not substantially change the findings for total fracture. Three large RCTs in community-dwelling individuals did not show reductions in the risk of fracture with CaD [Grant et al. 2005; Jackson et al. 2006; Porthouse et al.2005], and in meta-analyses including these RCTs, CaD marginally reduced the risk of total fracture (eight trials, n = 46,108, RR 0.87, 95% CI 0.77–0.97) [Tang et al. 2007], but did not prevent hip fracture [Avenell et al. 2009]. Thus, the findings of fracture efficacy with CaD in vitamin D deficient, frail, older women are not generalizable to other population groups or to the use of calcium monotherapy.Adverse Effects of Calcium Supplements
Until recently, it had been widely thought that, apart from causing constipation and gastrointestinal symptoms, use of calcium supplements did not cause adverse effects. The completion of these five large RCTs [Grant et al. 2005; Jackson et al. 2006; Porthouse et al. 2005; Prince et al. 2006; Reid et al.2006] of calcium or CaD has highlighted three potential adverse effects. In the Women's Health Initiative CaD trial (WHI CaD) with 36,282 women who were postmenopausal followed for 7 years, kidney stones occurred in 2.3% of participants and CaD increased the risk by 17% [Jackson et al. 2006]. Kidney stones were much less frequent in other trials, and incidence did not differ significantly between treatment groups [Grant et al. 2005; Prince et al. 2006; Reid et al. 2006]. In 1460 older women followed for 5 years, calcium monotherapy increased the risk of hospitalization for gastrointestinal disorder by 92%, and for acute abdominal pain by 81% [Lewis et al. 2012a]. Data on these adverse events are not available for other trials. The adverse events of most concern are cardiovascular events, more specifically myocardial infarction (MI) and stroke, which we will review in detail.Cardiovascular Effects of Calcium Supplements
Concerns about vascular effects from calcium supplements first emerged in the setting of renal impairment. In both dialysis and predialysis populations, calcium supplements accelerate vascular calcification and increase mortality [Block et al. 2007; Goodman et al. 2000; Russo et al. 2007]. However, it was not considered that these findings applied to the general population.Five years ago, we reported the first evidence for adverse cardiovascular effects of calcium supplements in healthy older women. The Auckland Calcium study was a 5-year RCT of calcium monotherapy in 1471 healthy women who were postmenopausal [Bolland et al. 2008; Reid et al. 2006]. The primary endpoint of the study was clinical fracture. Because of pre-existing evidence suggesting that calcium supplements have beneficial effects on cardiovascular risk factors such as hypertension [Griffith et al. 1999] and dyslipidemia [Denke et al.1993; Reid et al. 2002], we hypothesized that calcium supplements would decrease cardiovascular risk, and therefore cardiovascular events were prespecified as secondary endpoints in the trial protocol. To our surprise, there was a substantial increase in self-reported cardiovascular events in women randomized to calcium. In the calcium group, 31 women reported a MI compared with 14 in the placebo group (RR 2.24, 95% CI 1.20–4.17). For the composite cardiovascular endpoint of MI, stroke, or sudden death, the risk was also elevated with calcium (69 calcium group versus 42 placebo; RR 1.66, 95% CI 1.15–2.40). To ensure accuracy of these events, the medical records relating to all of these events were obtained and independently adjudicated, and a search for unreported events was undertaken using the national database of hospital admissions. The final results for verified events, including those unreported by participants, showed RRs for incident cardiovascular events with calcium ranging from 1.21 to 1.49, and increased rates of MI and the composite cardiovascular event ranging from 1.43 to 1.67. Although the size of the study and small number of cardiovascular events meant that the results were not definitive, they did flag cardiovascular risk as an important safety concern. However, further RCTs to explore the issue were not practical as the primary endpoint would be one of harm.
Limited data have been published on cardiovascular events in calcium studies, which led us to conduct a meta-analysis of unpublished cardiovascular data from existing RCTs. We invited the lead authors of 15 RCTs of calcium supplements in which the trial lasted for at least 1 year and had at least 100 participants to take part. Five provided patient-level data on cardiovascular events for 8151 participants with median follow up of 3.6 years, and 11 provided trial-level data for 11,921 participants with mean trial duration of 4 years. The results of these meta-analyses showed that calcium supplements increased the risk of MI by 27–31%, and there were smaller statistically nonsignificant increases in the risk of stroke (range 12–20%), the composite cardiovascular endpoint (12–18%) and mortality (7–9%) [Bolland et al. 2010a].
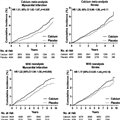
An important limitation of this meta-analysis was that the trials were restricted to calcium monotherapy, whereas the use of CaD was becoming more common in clinical practice. Previously, WHI CaD reported that CaD did not alter cardiovascular risk over 7 years in 36,282 women who were postmenopausal [Hsia et al. 2007]. An unusual feature of WHI CaD was that personal, nonprotocol use of the trial medications (calcium and vitamin D supplements) was permitted, and 54% of participants were taking personal calcium supplements at trial entry. We hypothesized that the widespread use of personal calcium in WHI CaD might have obscured an adverse effect of calcium on cardiovascular risk. We therefore reanalyzed WHI CaD comparing the effects of CaD on cardiovascular risk in nonusers and users of personal calcium. In the 46% of women not taking personal calcium, CaD increased the risk of cardiovascular events by 13–22%, whereas in the 54% of women already taking personal calcium supplements, CaD had no effect on cardiovascular risk [Bolland et al. 2011b]. The results of this reanalysis of WHI CaD were strikingly similar both in magnitude and temporal pattern to the results of our previous meta-analysis of calcium monotherapy (Figure 1). These results suggested that the widespread use of personal calcium supplements in WHI CaD had obscured the adverse cardiovascular effects of CaD.
 (Enlarge Image)Figure 1.
(Enlarge Image)Figure 1.Time to first event for myocardial infarction or stroke by treatment allocation in meta-analyses of five trials of calcium monotherapy (top panels) and in participants in the Women's Health Initiative (WHI) calcium and vitamin D trial not using personal calcium supplements at randomization (bottom panels) [Bolland et al. 2010a, 2011b]. Note the different scales on the y and x axes. HR, hazard ratio; CI, confidence interval.
We then pooled the data from women not using personal calcium in WHI CaD with all other existing RCTs of CaD for which cardiovascular data were available. In these four trials, CaD increased the risk of MI by 21% and stroke by 20% [Bolland et al. 2011b]. Because of the similarity between these results for CaD and the results for calcium monotherapy, we pooled the data from all the trials of calcium monotherapy and CaD to determine the effect of calcium with or without vitamin D on cardiovascular risk. Calcium/CaD increased the risk of myocardial infarction by 24–26% and stroke by 15–19% (Figure 2). Based on these meta-analyses, in 1000 people treated for 5 years, calcium/CaD would cause six additional heart attacks or strokes and prevent three fractures [Bolland et al. 2011b].
 (Enlarge Image)Figure 2.
(Enlarge Image)Figure 2.Meta-analyses of the effect of calcium supplements with or without vitamin D on cardiovascular events [Bolland et al. 2011b]. The left panels show the time-to-first-event analyses and the right panels random effects models of trial-level summary data when complete trial-level data were available. HR, hazard ratio; CI, confidence interval.
In the meta-analysis of calcium monotherapy, there was an interaction between dietary calcium intake and the risk of MI with calcium supplements when the cohort was divided by median dietary calcium intake [Bolland et al. 2010a]. However, when the cohort was divided by quintile of dietary calcium intake, there was no interaction and the risk of MI with calcium was similar in the groups with the lowest and highest calcium intake [Bolland et al. 2010a]. There was also no interaction between dietary calcium intake and the risk of stroke or the composite cardiovascular endpoint in this meta-analysis [Bolland et al.2010a], and no interaction between dietary calcium intake and cardiovascular events in WHI CaD [Hsia et al. 2007; Radford et al. 2013]. Therefore, the increased cardiovascular risk from calcium supplements appears to be independent of dietary calcium intake.
Criticisms
It is unsurprising that these unexpected findings have not been universally accepted, since calcium has been widely used for a long time and was considered safe. Similar resistance to accepting evidence that challenges dogma is well described [Prasad et al. 2012]. While criticisms have been made of our meta-analyses, few have been substantive, and we have extensively addressed the concerns raised [Bolland et al.2010b, 2011a, 2011c, 2011d, 2012; Reid et al. 2011a, 2011b]. Some criticisms have clearly been underpinned by commercial interests [Bolland et al. 2013b; Heaney et al. 2012]. Here, we address the main issues that continue to be raised.Several groups have chosen to highlight data from primary publications rather than using the data provided to us by the lead investigators and used in our meta-analyses [Bockman et al. 2012; Heaney et al. 2012; Rojas-Fernandez et al. 2012; Wang et al. 2010, 2012]. There is no reason that data published in a primary publication should take priority over other data from the same study, either unpublished or published elsewhere. The approach of only using data from primary publications is not consistent with recommendations of the Cochrane Collaboration and others, who repeatedly emphasize the importance of accessing and analyzing unpublished data [Easterbrook et al. 1991; Higgins and Green, 2008; Scherer et al. 2007]. Furthermore, the data in the primary publications are not directly comparable. For example, one study reported incident ischemic heart disease [Prince et al. 2006], another hospitalizations from cardiac disease and stroke [Baron et al. 1999], and another, the composite of MI, stroke, or sudden death [Bolland et al. 2008]. Some authors have simply pooled the risk estimates for these different endpoints and concluded that calcium supplements do not increase cardiovascular risk [Wang et al. 2010, 2012]. Such an approach is unwise because the data are not comparable, it is difficult to interpret the meaning of the pooled risk estimate, and it neither excludes nor invalidates the findings of increased risk for specific cardiovascular endpoints such as MI or stroke gathered in a standardized manner from the same trials.
The results of a secondary analysis of a RCT of calcium monotherapy [Lewis et al. 2011] are often contrasted with the findings of our metaanalyses. Indeed, the authors of the study described its findings as 'compelling evidence that calcium supplementation of 1200 mg daily does not significantly increase the risk of atherosclerotic vascular disease in elderly women' [Lewis et al. 2011] A number of issues with this study should be considered in its interpretation. The study is a secondary analysis of an existing RCT [Prince et al. 2006], although some appear to treat it as a separate study [Bockman et al. 2012; Rojas-Fernandez et al. 2012], and data provided by the authors on self-reported events were already included in our meta-analyses. For their secondary analysis [Lewis et al. 2011], the authors used the unadjudicated primary hospital discharge code. With this approach, there were only 28 MIs over 5 years in 1460 women of average age 75 years at baseline, an event rate approximately one-half to one-third the rate in women of similar age in two studies in our meta-analysis [Grant et al. 2005; Reid et al. 2006], and similar to the rate in women 12–16 years younger in two other studies in the meta-analysis [Baron et al. 1999; Hsia et al. 2007]. The low event rate suggests that a number of MIs have been missed. Therefore, these results do not provide strong evidence for the cardiovascular safety of calcium supplements both because the study lacks sufficient power to detect between-group differences in event rates of the magnitude observed in our meta-analyses and because there is evidence of missing events. Finally, updating the results of our meta-analyses using these new data does not change the results (Table 1).
Some authors have incorrectly suggested that including self-reported events in our meta-analysis invalidates the results [Bockman et al. 2012; Heaney et al. 2012; Lewis et al. 2012a, 2012b; Lumsden, 2012; Medicines and Healthcare Products Regulatory Agency (MHRA), 2011; Nordin et al. 2011; Rojas-Fernandez et al. 2012]. In our patient-level meta-analysis of calcium supplements used as monotherapy [Bolland et al. 2010a], only 23% of MIs were from unverified self reports. The remaining 77% were ascertained from hospital discharge data (15%), or death certificates (41%), or were independently adjudicated (22%). For our patient-level meta-analysis of calcium supplements with or without vitamin D [Bolland et al. 2011b], only 9% of MIs were unverified self reports, with 6%, 16%, and 68% obtained from hospital discharges, death certificates, and independent adjudication respectively. Table 1 shows the result of excluding self-reported events from our analyses: for calcium with or without vitamin D the relative risk for MI was 1.26 (95% CI 1.08–1.48, p = 0.004), and for stroke it was 1.18 (95% CI 1.01–1.38, p = 0.038). Thus, exclusion of self-reported events does not alter the finding of increased cardiovascular risk from calcium supplements.
Several criticisms of our reanalysis of WHI CaD have been raised, although our analyses frequently appear to be misinterpreted and misunderstood. Some critics have claimed that the rationale for our reanalysis of WHI is incorrect [Bockman et al. 2012; Heaney et al. 2012; Lewis et al. 2012b; Lumsden, 2012; MHRA, 2011]. We hypothesized that the widespread use of nonprotocol personal calcium supplements may have obscured the effects of CaD on cardiovascular events because, for the majority of participants, the trial compared higher doses of calcium with lower doses of calcium rather than comparing calcium with placebo. This hypothesis was endorsed by the British Medical Journaleditorialists [Abrahamsen and Sahota, 2011]. It is not possible to draw inferences on the effects of calcium compared with placebo on cardiovascular risk from a trial design that compares cardiovascular risk between women taking higher dose calcium and lower dose calcium. To compare the effects of coadministered CaD with placebo, we reanalyzed WHI CaD restricting the analysis to women not taking personal calcium supplements. This analysis showed increased cardiovascular risk from CaD. For the women already taking calcium supplements at baseline, the comparison of higher dose calcium supplements versus lower dose calcium showed no difference in cardiovascular risk from CaD, suggesting no dose–response relationship. Thus, women taking lower doses of calcium supplements have similar cardiovascular risk to those taking higher doses, and this risk is elevated compared with women not taking calcium supplements. Recently the WHI investigators have reanalyzed their data using the same approach, obtaining similar results [Prentice et al. 2013].
Some have suggested that confounding might explain the findings of increased cardiovascular events in women not taking personal calcium, because the subgroup of women using personal calcium supplements differed from the subgroup not using these supplements [Heaney et al. 2012; Lumsden, 2012; Rojas-Fernandez et al. 2012]. This interpretation is not likely, as there were no baseline differences between treatment groups within each subgroup defined by personal calcium use, and there were no consistent interactions between cardiovascular events, treatment allocation, and other variables in the entire WHI cohort [Hsia et al. 2007] or in the women not using personal calcium [Radford et al. 2013]. Some have suggested that the WHI reanalysis findings should be dismissed because not all of the observed increases in cardiovascular risks were statistically significant [MHRA, 2011; Prentice et al.2013]. Even with its large sample size, WHI did not have sufficient power to detect small differences (<30%) in incidence of some endpoints between treatment groups. The WHI results should not be considered in isolation when there is a body of other RCTs showing very consistent results. When the data from these RCTs are pooled, these meta-analyses have adequate power to detect very small (<15%) differences in incidence between treatment groups.
Lastly a number of authors have focused on mortality endpoints. Some have inappropriately emphasized a finding of reduced mortality from CaD only in the subgroup of women taking personal calcium at baseline [Abrahamsen and Sahota, 2011; MHRA, 2011]. This interpretation is not consistent with recommended approaches to subgroup analyses [Assmann et al. 2000; Lagakos, 2006; Yusuf et al.1991]. Since the formal interaction test between personal calcium use, CaD allocation and mortality was not statistically significant, the result is most likely a false positive. Others have suggested that because the increases in cardiovascular risk did not translate into increased mortality, the findings are either spurious or not clinically relevant [Lumsden, 2012; MHRA, 2011; Wang et al. 2012]. This interpretation is concerning as it suggests that nonfatal MIs and strokes are clinically unimportant. It is not consistent with interpretation of trials of other agents in which increases or decreases in cardiovascular event rates are accepted as valid despite no statistically significant effects on mortality [Anderson et al. 2004; Nissen and Wolski, 2007; Rossouw et al. 2002; Steering Committee of the Physicians' Health Study Research Group, 1989]. It also overestimates the impact that a 15– 25% increase in risk of MI or stroke would have on all-cause mortality. In our reanalysis of WHI, only 145/712 women who sustained a MI or stroke died before the end of the study, and 80 of these 145 deaths were attributed to cardiovascular causes. If calcium/vitamin D use caused a 20% increased risk of MI/stroke, and this translated into a 20% increased risk of cardiovascular mortality, there would have been about eight extra cardiovascular deaths in the calcium/vitamin D group during the trial. A difference of this magnitude would have had minimal impact on either cardiovascular or all-cause mortality.
Later Studies
Since the publication of our most recent metaanalysis, the results from only one relevant RCT have been published. This was a RCT of sunlight exposure to raise vitamin D levels of Australian rest homes residents, and reported that the addition of calcium supplements to sunlight exposure was associated with increases in all-cause and cardiovascular mortality [Reid et al. 2011b; Sambrook et al. 2012].A number of observational studies of cardiovascular risk and calcium intake have been published during this period. Such analyses must be regarded with caution because observational studies can only generate hypotheses, not test them, and their value is debatable when there is a large body of data from RCTs to draw upon. Furthermore, the studies have used a variety of methods to estimate dietary calcium intake, such as a single 24 h dietary questionnaire [Van Hemelrijck et al. 2013], multiple food frequency questionnaires [Michaelsson et al. 2013], and a food-frequency questionnaire for the past year [Xiao et al. 2013]. The precision of the estimates of calcium intake is likely to vary, which may contribute to differences in study results. Nevertheless, these studies have received a lot of publicity, probably because of the large number of participants. Collectively, they have reported increased rates of MI [Li et al. 2012, 2013], coronary heart disease [Pentti et al. 2009], stroke [Li et al. 2013], cardiovascular death [Xiao et al. 2013], and mortality [Michaelsson et al. 2013] in users of calcium supplements. Even in ostensibly negative studies, results consistent with cardiovascular harm from calcium have been reported. For example, in the National Health and Nutrition Examination Survey III cohort, the risk of fatal acute MI in those taking 500–1000 mg/day of calcium supplements was 1.23 (95% CI 0.53–2.82), and for those taking 1000–2000 mg/day the risk was 1.15 (0.37– 3.54) [Van Hemelrijck et al. 2013]. Neither result was statistically significant, but these results were based on only 362 out of 16,844 deaths and the study did not have sufficient power to detect differences in event rates of less than 30%. These results highlight that even apparently large observational studies may not have sufficient power to detect small differences in event rates for deaths due to ischemic heart disease or for more specific cardiovascular endpoints.
Most recently the European Medicines Agency reported that strontium ranelate increased the risk of MI (RR 1.6, 95% CI 1.07–2.38) in a pooled analysis of around 7500 participants in RCTs of osteoporosis [MHRA, 2013]. Strontium is a divalent cation with many similar chemical and biological properties to calcium, and binds to the calcium receptor [Brown, 2003]. Given these similarities, as well as similar effects on both fractures and cardiovascular events [Bolland et al. 2013a], it seems possible that the same underlying mechanism might explain the increased cardiovascular risk for strontium and calcium.
Possible Mechanism
The cause of the increased cardiovascular risk from calcium supplements remains unclear, but potential mechanisms have been extensively reviewed [Reid et al. 2010]. The finding of increased cardiovascular risk from calcium supplements but not dietary calcium intake in most observational studies [Al-Delaimy et al. 2003; Ascherio et al. 1998; Bostick et al. 1999; Iso et al.1999; Knox, 1973; Li et al. 2012; Van der Vijver et al. 1992; Van Hemelrijck et al. 2013; Xiao et al. 2013] but not all studies [Michaelsson et al. 2013] has led to the hypothesis that the rapid and sustained increases in serum calcium after ingestion of a calcium supplement may have a central role.Impact Upon Calcium Prescriptions
Figure 3 shows that there has been a 67% reduction in prescriptions for calcium in New Zealand since the publication of our RCT in 2008. Similar published data are not available for other countries, but we are aware of smaller reductions in calcium use in Europe and the USA.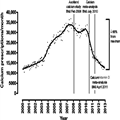 (Enlarge Image)Figure 3.
(Enlarge Image)Figure 3.Number of prescriptions for calcium supplements per month in New Zealand from 2000 to 2013. The solid line is a smoothed average of the individual points (data provided by Robert Hipkiss, Ministry of Health, New Zealand).
Implications for Practice
Some authorities have recommended that more focus be placed on dietary calcium rather than calcium supplements. Worldwide, there are substantial differences in calcium intake, with higher intakes in Western countries and lower intakes in Asia and Africa. No RCTs have assessed the effect of increasing dietary calcium on fracture incidence or cardiovascular events. While observational studies have addressed these issues, their interpretation is often difficult because causality cannot be inferred, confounding is difficult to assess and control for, and the total calcium intake of people taking calcium supplements is usually much greater than the intake from diet alone. With these limitations, most [Al-Delaimy et al. 2003; Ascherio et al. 1998; Bostick et al. 1999; Iso et al. 1999; Knox, 1973; Li et al. 2012; Van der Vijver et al. 1992; Van Hemelrijck et al. 2013; Xiao et al.2013] but not all [Michaelsson et al. 2013] observational studies have shown no association between dietary calcium intake and cardiovascular events. With regard to fracture, at a global level, there is little evidence that countries with low calcium intake have high fracture incidence [Kanis and Passmore, 1989] and observational studies also do not suggest that levels of calcium intake are associated with risk of fracture [Bischoff-Ferrari et al.2007; Cumming et al. 1997; Warensjo et al. 2011]. Therefore, current evidence suggests that dietary calcium intake does not require close scrutiny for the majority of people.At the population level, any effects of calcium supplements on fracture risk are outweighed by the increased cardiovascular risk. Likewise, at an individual level, the increased cardiovascular risk will generally outweigh any benefits on fracture prevention. Therefore, the widespread use of calcium supplements to improve bone health should be abandoned. Although there is clear evidence of fracture prevention with CaD in institutionalized frail older women with a high prevalence of vitamin D deficiency, there is also evidence that the addition of calcium supplements to sunlight exposure increases mortality in this population. Thus, the balance of risk and benefit in institutionalized older people currently remains uncertain, but vitamin D supplements can be used independently of calcium. Patients who are at high risk of fracture should be encouraged to take agents with proven efficacy in preventing vertebral and nonvertebral fractures. Calcium supplements are often administered with such agents. However, antiresorptive agents administered without calcium supplements prevent fractures [Anderson et al. 2004; McCloskey et al. 2007; Rossouw et al. 2002], the magnitude of effect of antiresorptive agents on bone density in trials without calcium [Bonnick et al. 2007; Grey et al. 2009, 2012; Hosking et al. 1998] is similar to trials in which calcium is coadministered, and the effect of the antiresorptive zoledronate was similar in women with high or low calcium intake [Bourke et al. 2013]. Thus, there is little evidence to suggest that antiresorptive agents need to be coadministered with calcium supplements to be effective.
